Fecal Microbiota Transplants (FMT)
Everything you need to know about Fecal Microbiota Transplants (FMT). Stool donors, screening, procedures, where to get FMT, safety, outcomes, and more.
HumanMicrobes.org is trying to find the fewer than 0.1% of people who qualify to be a highly-effective stool donor.
Table of Contents
Screening:
FMT stool donor screening questionnaire -- FMT is only as safe as your donor is healthy.
Do not solely rely on testing, whether it be conventional, 16s, shotgun metagenomics, or anything else, as it is very limited in value. More on testing: https://humanmicrobiome.info/testing
These two sets of guidelines can be used for basic blood & stool testing, but they cannot determine donor safety on their own:
- International consensus conference on stool banking for faecal microbiota transplantation in clinical practice (Nov 2019) https://gut.bmj.com/node/226914.full#boxed-text-2
- European consensus guidelines tests (Mar 2017): https://gut.bmj.com/content/66/4/569#boxed-text-3
Donor quality seems to be the key for antibiotic-resistant pathogens, and for COVID.
If you cannot find a participating doctor, the blood tests can be ordered directly from various online sources, such as https://requestatest.com/ or https://www.ultalabtests.com/Patient. In the UK you can use https://www.medichecks.com.
For the stool testing portion you can use https://www.mymedlab.com or https://mylabsforlife.com to get the Diagnostic Solutions GI Map test.
In the EU you can try https://ifu-wolfhagen.de/ or https://smartnutrition.co.uk/ or http://www.nordiclabs.com/EDetail.aspx?id=3827 to get the GI Map.
If you look at their Sample Report, it has most of the recommended stool tests. If you get this test through a provider you need to specifically ask them to check off on the order the "beta-lactamase resistance" section, or "Antibiotic Resistance Genes, genotypes". Mymedlab said "when you receive your kit, you can make the change on the requisition form".
Some of the blood testing can typically be done at a free STD clinic. https://gettested.cdc.gov/
Thepowerofpoop.com recommends Direct Labs - the "Labs for Fecal Diversity Tests Only" aren't that useful in my opinion (see the "testing" section of this wiki). The "Comprehensive Digestive Stool Analysis 2.0™ (CDSA 2.0)-Genova Kit" is probably the most useful directlabs test.
A few things to keep in mind when looking for a donor:
- The gut microbiome is heritable and gets passed down generationally. Including dysbiosis, pathogens, and extinctions from poor diet and antimicrobials. A child with no lifetime antimicrobial use may not actually have an eubiotic, disease resistant gut microbiome, but rather they may have just not yet been exposed to an infectious pathogen that necessitated an antimicrobial.
- There are differences between everything -- sex, race, ethnicity, lifestyle, location, etc. There is little to no evidence those differences (other than health-related ones, such as healthy diet and healthy lifestyle) matter for safety or efficacy. Current evidence supports universal donors. The Impact factors and Donor-recipient matching sections have more info.
- Relatives can often have "pre disease" states of dysbiosis [1][2]. Meaning they have dysbiosis themselves but not yet enough to trigger the disease of the family member that needs the transplant. So contrary to common misinformation, relatives are often not ideal. The EU consensus concluded universal donors are as good as any. And that is supported by this recent IBS clinical trial and this Mar 2020 systematic review.
- Both genetic and gut microbiome diversity are beneficial.
- There is a large amount of evidence (in this wiki) that donor quality (rather than compatibility) is the #1 factor. But of course each donor (and recipient) is very unique and thus some donors would have certain microbes needed to treat certain conditions/individuals, while others do not. And naturally there would be varying results when transplanting one unique microbiome into another. I compared it here to a jigsaw puzzle.
- Nearly anything wrong with a donor can be transferred via FMT [1].
- Donors often misjudge their stool quality. So you probably want to get a daily sample for a few days in a row before using any of it, just to judge the quality and consistency yourself. If a person is having unstable stools it's probably not safe.
- You absolutely can not blindly trust donor quality from official sources such as stool banks, clinical trials, hospitals, etc. [1]. You must learn what it means to be a high quality donor and verify that the provided donor is high quality. If they will not verify that information with you, do not use them.
What healthy poop looks like: Bristol stool chart.
Soft stools seem to be from one or more of:
- A low quality gut microbiome that lacks certain microbes needed in the digestion of certain foods. Or lacks certain microbes that control/limit others.
- A pathogen that feeds off certain food items (iron for example), and thus causes soft stools & other problems when eating those foods.
- Temporary stomach upset from either mild food poisoning or poor hygiene/sanitary practices.
When starting out, I had no idea how important stool type & consistency was, but it seems that high-quality donors have identical stools, while low-quality donor's stools are heterogeneous. Thus, it's one of the main ways to judge donor quality. This Anna Karenina hypothesis supports this. As do the majority of case reports I've seen, and this study [1].
This 2017 study saying otherwise is only for c.diff (which requires much less strict donor criteria). And it's quite likely (looking at the donor criteria) that studies like that lacked high quality donors, so they may have only been comparing average/low quality donors with each other. Also I believe it is a matter of "the highest quality donors all have type 3 stools, but not every type 3 stool donor is high quality".
Currently, I believe it's likely that deficiencies in bile acid metabolism (missing microbes) is a primary cause of stool types other than dark type 3.
The 4 basic steps to donor screening (in this order):
- A detailed questionnaire.
- Verification of stool type and physical fitness. Stool type should be verified over at least 5 consecutive days.
- If it's not already someone you know well you should do a video or in-person interview. Try to get to know them a bit.
- Stool & blood testing.
More info on what donor quality means, and why it's so hard to find high quality donors: https://forum.humanmicrobiome.info/threads/donor-quality-and-stool-type-hypothesis-for-fmt-fecal-microbiota-trans.142/
See the "impact factors" section under "scientific info" heading for more on donors, including supporting evidence for athletes.
Detailed experiences & lessons from 13+ different stool donors (2018- ).
Procedure:
Check out the video on this page for a good overview of ASU's recent FMT study, which was one of the best I've seen: https://autism.asu.edu/ - they used both oral and rectal routes.
The most common/major flaws with FMT studies/procedures are:
- Poor donor quality [1][2][3][4][5][6]. Donors should be under 30 [1][2][3], have very limited life time antibiotic exposure (ideally none) [1], athletic & low body fat, and good mental health. Firm stool consistency seems important too. Typical donor criteria you see is a complete joke. Stuff like "no abx in past 3 months, 18-50 yrs old, no pathogens in stool & blood test".
- Insufficient treatment length. Many studies only do a single infusion, but for many people/conditions you might need to do it daily for 2+ months (Eg: ASU autism study).
- Too much oxygen exposure. Blending is quite common and this oxygenates the stool sample.
- Colon-only procedures. The small intestine is very important [1], so completely ignoring it is a likely flaw for some conditions [1].
Keep in mind that c. diff is a lot easier to cure than other conditions. So even though a study shows 'x' is effective for c.diff, other harder to cure conditions will likely need stricter criteria.
It's common for the recipient to feel feverish & chills, and possibly some initial diarrhea & other temporary side effects after the first 1-2 FMTs. It seems to be a sign of a high quality donor. Symptoms of a "changing of the guard".
The less delay between the donor having the BM and the recipient using it, the better. 15 minutes or less might be ideal, but it can be hard to always be there when your donor has a BM, so it's possible to use an insulated lunch bag like this:

with ice packs & ziplock freezer bags in it that the donor keeps with them during the day. Then just make sure to flatten the air out before zipping it shut and putting it back in the ice bag.
Freezing the stool for either shipping or storage is common. Typically, a cryoprotectant is added to protect the microbes from freezing damage. This may not be necessary (see Freezing section below).
Glycerol/Glycerin is the commonly used antifreeze additive, but it's also a laxative, and therefore problematic for some people. A maltodextrin-trehalose (MD-TR) mixture is a good alternative. Maltodextrin can be bought in bulk online for around $4/lb. And trehalose can be bought for around $10/lb. The ratios used in that study were approximately 3 tbsp maltodextrin + 1 tbsp trehalose + 100mL (7 tbsp) saline. That MD-TR-saline mixture can then be added to stool at a 4:1 ratio. 4g of the mixture with 1g of stool.
This may be too watery for your purpose. If so, you can reduce the amount of saline added. The saline is only used to create the desired consistency so that it mixes well with the stool. The MD-TR is what protects the microbes in the stool. 1 part saline to 2 parts MD-TR should result in a mixture close to the consistency of glycerol. You can then mix that in with the stool until you get the consistency you want.
Alternatively (but probably less ideal), you could mix in a little bit of saline (close to ½ tbls saline per 1 tbls stool), little by little, mixing them in the ziplock bag the stool was collected in, to create a thick yogurt/custard-like consistency, then add MD-TR till it's a doughy/firm consistency, which can then be encapsulated or frozen straight.
UPDATE: Here's a video demonstration https://www.youtube.com/watch?v=89FCAsqC8BY for making capsules, and mixing in the powder antifreeze. I found it difficult to mix the powder in well at the end, but I used a substitute powder, and MD-TR mixes much easier.
Using glycerol is a bit more simple since it's a thick liquid. You can just pour it into a bag with the stool till you have the consistency you want, but this is not recommended due to the laxative effect. The recommended amount is 10-15% of the final concentration. Eg: ½ cup saline, 2 tablespoons stool, 2 tablespoons glycerol.
But again, that amount of saline is way too much. So you can follow this video demonstration where a 1:1 ratio of glycerol:stool is used, and saline is only added as needed.
When adding liquid, saline should be used instead of pure water. Saline provides osmotic protection for microbial cells, helping to maintain cell integrity and viability.
To create saline: Add ½ teaspoon of non-iodized salt (iodine is anti-microbial) to 1 cup of filtered or distilled water (no chlorinated water). Or 1 teaspoon of salt for 2 cups of water.
Treatment length:
Length is unknown and depends on the condition being treated, procedure quality, and donor quality. For IBS for example, as little as one enema has been reported to be effective for some people, but others with IBS report needing many more over many months. For the recent ASU autism study [1,2] daily oral FMTs were done over a period of 10 weeks, and gradual improvements were seen throughout, which suggests that 10 weeks or longer might be necessary in some cases. However, there were many procedure & donor deficiencies in their study, so treatment length should decrease if one is able to rectify those deficiencies.
El-Salhy's highly effective 2019 IBS FMT trial only did a single 30-60g dose to the distal duodenum via the working channel of a gastroscope.
For CDI (Clostridium difficile infection): "A single FMT was needed in 30 (52.6%) patients, 2 FMTs in 16 (28.1%) patients, 3 FMTs in 4 patients (7%), and 4–5 FMTs in 2 (3.5%) patients to achieve clinical cure" (2016) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5479393/
Sep 2020 (n=54) study showing 2 consecutive FMTs achieves 98% cure rate for C. diff, and cites other studies showing more FMTs = higher cure rates: https://link.springer.com/article/10.1007/s40121-020-00339-w
"periodic and repetitive FMT is required for a sustained effect" (Jul 2021, n=227) https://www.frontiersin.org/articles/10.3389/fmed.2021.710452/full Long-Term Follow-Up Results of Fecal Microbiota Transplantation for Irritable Bowel Syndrome: A Single-Center, Retrospective Study.
Upper vs lower routes:
Upper, also known as "top-down" or oral, can be done directly, or via capsules, or via naso tube.
Lower/rectal route, can be done via deep retention enema, or colonoscopy.
Lower-only is possibly inferior to capsules because it only gets the colon, which is a small part of the entire digestive system.
With the oral route, some people have concerns about stomach acids & bile killing off sensitive microbes before they make it to the colon. But various studies below indicate little to no difference. Personally, I found that with certain donors it seemed that lower-route was more effective, but I also experienced lower-route to be generally harmful with multiple donors, so I stopped doing it. Other people have reported that oral seemed more effective for them. So I would recommend trying both routes if possible. I later experimented with upper vs lower and discovered that lower-only was incomplete.
Effect of Oral Capsule– vs Colonoscopy-Delivered Fecal Microbiota Transplantation on Recurrent Clostridium difficile InfectionA Randomized Clinical Trial (2017, n=116) https://jamanetwork.com/journals/jama/fullarticle/2664458 "Among adults with RCDI, FMT via oral capsules was not inferior to delivery by colonoscopy"
The 2017 ASU Autism study tested both routes and found no difference. https://autism.asu.edu/
"The response rate was significantly higher in the SI (small intestine) and repeated SI groups than in the LI (large intestine) group. IBS symptoms at 2 years after FMT were less severe in the SI and repeated-SI groups than in the LI group" https://www.sciencedirect.com/science/article/abs/pii/S1286457924001084 Factors underlying the Long-term Efficacy of Faecal Microbiota Transplantation for Patients with Irritable Bowel Syndrome (Jun 2024)
March 2019 review of FMT for c.diff in Germany shows that lower route alone has a higher cure rate than upper alone, both together have the highest cure rate, but the results were confounded by age so the authors think there's no difference. Chart image.
March 2020 systematic review of c. diff concludes FMT cure rates were colonoscopy 94.8%, capsule 92.1%, enema 87.2%, and NGT/NDT (naso tube) 78.1%.
Sep 2022 analysis of 269 C. diff patients concluded "FMT using freeze dried capsules has a similar safety and effectiveness profile compared to colo-FMT, without the procedural risks of colonoscopy"
Lower endoscopic delivery of freeze-dried intestinal microbiota results in more rapid and efficient engraftment than oral administration (Feb 2021, 27 c. diff patients) https://www.nature.com/articles/s41598-021-84152-6
Lower-only was effective for Crohn's disease Feb 2023, n=25, multiple FMTs, 72.7% clinical remission
March 2021 study showed that both routes together was more effective than either-or: https://www.dldjournalonline.com/article/S1590-8658(21)00090-6/fulltext
Sep 2022, meta-analysis - "Our results provide further support for administering FMT by combined routes" https://web.archive.org/web/20220917205431/https://old.reddit.com/r/HumanMicrobiome/comments/xgkmk2/two_slightly_conflicting_fmt_meta_analyses/
The Efficacy of Faecal Microbiota Transplant and Rectal Bacteriotherapy in Patients with Recurrent Clostridioides difficile Infection: A Retrospective Cohort Study (Oct 2022, n=343) https://www.mdpi.com/2073-4409/11/20/3272/htm "FMT capsules were more effective than both FMT enema and RBT; 79.9% in the FMT capsule group, 53.3% in the FMT enema group, and 61.8% in the RBT group"
Factors affecting the outcome of fecal microbiota transplantation for patients with irritable bowel syndrome (July 2023, n=186) https://onlinelibrary.wiley.com/doi/10.1111/nmo.14641 "Administrating transplant to the small intestine had a long-term higher response rate than that administrated to the large intestine, and led to long-term colonization of beneficial bacteria"
Fecal Microbiota Transplantation in Children with Autism (Dec 2024, n=98) https://forum.humanmicrobiome.info/threads/fecal-microbiota-transplantation-in-children-with-autism-dec-2024-n-98.755/ Capsules, nasal tube (NJT), endoscopic tube (TET). "Upper route may be more effective and safe"
OpenBiome, the main US stool bank (c.diff only) offers all 3 methods (enema, naso tube, capsules): https://www.openbiome.org/fmtcapsules/ - https://www.openbiome.org/clinical-guidance
For worries about SIBO see the SIBO section below.
Some links and discussion regarding route and method safety: https://archive.is/JRWmc - https://archive.is/0fNsW
For more, see "Safety" section below.
Before the procedure:
Depending on the condition, it might be helpful to take an antibiotic (for at least a few days, but they're typically prescribed for 1-2 weeks I believe) in order to clear out the current microbes so the new ones have an easier time to establish themselves [1][2][3][4][5]. But the evidence for most conditions isn't here yet, and antibiotics can have a wide range of severe, long term detriments, and there's quite a bit of other evidence below showing antibiotics before hand are no better or worse.
For:
Strain-resolved analysis in a randomized trial of antibiotic pretreatment and maintenance dose delivery mode with fecal microbiota transplant for ulcerative colitis (Apr 2022, n=22) https://www.nature.com/articles/s41598-022-09307-5 "Of patients who received antibiotic pretreatment, 6 of 11 experienced remission after 6 weeks of treatment, versus 2 of 11 non-pretreated patients. Patients assigned to ABX + arms were pretreated with neomycin, vancomycin and metronidazole 500 mg twice-daily for 5 days, followed by a one-day wash-out period. Patients then underwent colonoscopy. Starting one week later, and over the next six weeks, patients received maintenance doses, 30 capsules weekly, or a 60-mL enema weekly. Donor stool was provided by OpenBiome"
Identification of clinical and ecological determinants of strain engraftment after fecal microbiota transplantation using metagenomics (Aug 2022) https://www.cell.com/cell-reports-medicine/fulltext/S2666-3791(22)00254-3 "comprehensive fecal metagenome analysis of 14 FMT trials, involving five pathologies and >250 individuals. Donor strain engraftment was enhanced through antibiotic pretreatment and bowel lavage"
Against:
This 2010 rat study showed antibiotic intake prior to transplantation did not increase establishment of the donor phylotypes. It also showed that broad-spectrum antibiotics do not "wipe everything out, letting you start from a clean slate", but rather antibiotics only temporarily suppress certain types and allow others to increase, but after antibiotic cessation, bacterial load generally returns to the previous state, but diversity seems reduced for the long-term, including after FMT. [1]. - "Clearly, host factors also play a role in shaping the intestinal microbial ecosystem, and those factors might be also altered by antibiotic intake". "Although this finding makes ecological sense, that antibiotics might be almost as deleterious to the input community as to the endogenous community, is a highly counterintuitive result that should be taken into account in designing future bacteriotherapy protocols".
A conflicting result using human-to-mouse FMT with and without abx [1], and some discussion on possible reasons for the difference.
Another 2019 mouse study (STAMP) showed 3 out of 4 antibiotics (vancomycin, cefotaxime, metronidazole) used for pre-treatment "resulted in impaired transplantation efficacies". The 4th antibiotic (polymyxin) seemed to help colonization: https://www.nature.com/articles/s41467-019-09267-x
"A recent multicenter study of ulcerative colitis patients who received SER-287 (Seres Therapeutics), a microbiome-based therapy composed of a consortium of bacterial spores. Initially, the trial used vancomycin pretreatment, but the researchers found that it did not improve the results" (Jan 2019): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6423689/
"specific preparation of the patient using an antibiotic induction regimen, proton pump inhibitors, or antimotility agents did not impact treatment success" (Mar 2019) https://journals.sagepub.com/doi/10.1177/2050640619839918
"Pre-treatment with antibiotics before FMT did not have any significant impact on clinical outcomes in IBS-D patients" (June 2019) https://www.healio.com/gastroenterology/irritable-bowel-syndrome/news/online/%7Bb7ea1e6f-d12c-4b81-9978-2f0d64528018%7D/oral-fmt-with-antibiotics-does-not-improve-symptoms-of-ibs-d
Pretreated with ciprofloxacin and metronidazole for 7 days and still got poor results for UC (Jul 2021) https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-021-01856-9
Effect of antibiotic pretreatment on bacterial engraftment after Fecal Microbiota Transplant (FMT) in IBS-D (Jan 2022, n=44) https://www.tandfonline.com/doi/full/10.1080/19490976.2021.2020067 "antibiotic pretreatment significantly reduced bacterial engraftment after FMT in patients with IBS-D"
Fecal Microbiota Transplantation Versus Vancomycin for Primary Clostridioides difficile Infection: A Randomized Controlled Trial (Jun 2025, n=104) https://forum.humanmicrobiome.info/threads/fecal-microbiota-transplantation-versus-vancomycin-for-primary-clostri.1084/ "Clinical cure with no recurrence seen in 67% for FMT vs 61% for vancomycin. Up to 78% for FMT with additional treatment"
Study in C. Diff patients using FMT as first-line treatment (instead of only after antibiotics fail) gets 98% cure rate (Sep 2020, n=54): https://archive.vn/QtQlM. It cites this 2012 pooled analysis (n=289) that found no difference in cure rates between antibiotic-treated or non-antibiotic.
If you take antibiotics prior you are making a bet that the donor will restore everything the antibiotic kills off/damages. Two mouse studies showed FMT may not completely restore immune function damaged by antibiotics: (2017), (2018). And this May 2020 mouse study showed that FMT was unable to reverse the microbiome changes from antibiotics - "we found that control mice did not restore disturbed microbial communities. Instead, mice with disturbed microbial communities induced disturbance in control mice"
Neither Xifaxan nor Flagyl made low quality donors more effective for me. Certain conditions where a pathogen is a primary cause are more likely to benefit from antibiotics, but due to severe limitations in testing it can be hard to identify those individuals and the right antibiotic for them.
A clinic in Melbourne Australia gives Xifaxan 500mg 2x/day for 10 days, Flagyl 400mg 3x/day for 10 days, Nystatin 1 capsule 3x/day for 10 days prior to their FMTs: https://web.archive.org/web/20190611185139/http://www.melbournefmt.com.au/fmt_procedure.html
Xifaxan only targets the small intestine [1][2] and thus may not be a good choice for cases of dysbiosis that are primarily in the colon. 2017 study showed little to no benefits from Rifaximin pre-treatment for UC [1].
I read somewhere that a Florida clinic (RDS Infusions) is giving Neomycin for 7 days prior to FMT.
You could also consider doing a colonoscopy prep/bowel cleanse [1], which includes inducing diarrhea to clear out the entire intestinal tract, but personal experience says it's not more effective than just doing the retention enema after a regular BM. Though inducing diarrhea itself may have some impacts, good or bad [1][2][3][4][5][6][7]. 2022 study of 11 people showed bowel prep for colonoscopy only had temporary impacts [1].
FMT via lower-route with no bowel prep was effective for Crohn's disease Feb 2023, n=25, multiple FMTs, 72.7% clinical remission.
FMT via upper-route with no bowel prep was effective for IBS El-Salhy, 2019, n=165.
Taking a bunch of multi-strain probiotics prior did not seem to have any benefits for me, and this 2018 study showed it can result in an increased rate of infection [1].
PPI (proton pump inhibitor) use is not currently supported [1].
This 2021 study showed no benefit from fasting beforehand. Discussion on fasting & FMT: https://archive.ph/PBWKa
Upper route:
Here's a video demonstration https://www.youtube.com/watch?v=89FCAsqC8BY for making capsules.
Using quick release capsules (Size 000 - largest possible: 1, 2) gets the entire digestive system. Using slow release (enteric coated) capsules still gets most of the small intestine and avoids stomach acids that may reduce some microbe counts.
For me it seems like with quick release methods, taking small amounts (maybe 10-15 capsules depending on their size, 1oz or less) on an empty stomach (2-3 hours after a meal or ½-1 hour before a meal) first thing in the morning with lots of water is more effective than taking it with a meal. Even when the meals contained prebiotics. This is likely due to various digestive system secretions triggered by meals (including large amounts of stool). Enteric coated capsules could be better, but I don't think an FMT study has done a comparison, nor have I seen anyone else report doing a comparison. I tried double encapsulated, delayed release vegan capsules, and it didn't seem noticeably better.
If the womb is sterile, virtually all microbes in a donor's stool would have gotten into the donor's colon via the donor's mouth first. So microbes that are evolved to thrive in the human gut should be able to make the trip from the mouth to the colon. Most probiotics are not human-sourced/human-native, so studies showing probiotics not making it through stomach acid aren't reliable for this.
Size 00 enteric coated: https://www.amazon.com/gp/product/B06XGM6HK9
Optionally, you can use two sizes of capsules and double encapsulate.
How to:
Donor poops in ziplock bag:

Then ASAP (within a few minutes) the stool is put in capsules, and capsules are swallowed. Using a 60ml Catheter Tip Disposable Syringe like this might be the easiest way:

You can shovel the whole stool into the syringe without any dilution. You may have to cut off the tip of the syringe and widen the opening by stretching the plastic with a sterilized nail. And keep some toothpicks on hand to unclog the opening.
Without the syringe, a toothpick used as a shovel worked fine for me (about 20 capsules in ~10 minutes). A fast food straw split down the middle making a canoe shape might be a little better.
Another method is to snip the corner off the bag:

And squeeze into capsules similar to how you apply frosting:

Local stores (arts & crafts like Michaels, supermarkets, etc.) should have icing piping nozzles of various sizes that would work well.
That's a two handed method that might require a capsule-holding tray. Make sure the tray matches the sizes of your capsules.
If you can stomach it you can skip the capsules and just straight up swallow the poop. As a plus side, unhealthy poop is going to be a lot more repugnant (some support: [1][2]). And if the stool is too soft it will melt the capsules anyway. You could also add water/saline and use a straw to drink the liquid.
In ASU's 2017 FMT Autism study they used the oral route (filtered out most of the large particles so no taste, and then mixed it in with liquids that the patients drank) in some patients and rectal in others and found no differences.
Lower route:
Donor poops in ziplock bag

Saline is added (you can eyeball the amount. Make it watery enough to flow through the colon easily), mix gently (so as not to oxygenate the liquid) with hand from outside the bag, do enema (enema, not colonoscopy - IE: only needs to go in an inch or so) with wide-ended (so stool doesn't get stuck) turkey baster:

Use lube.
I use the knee-chest position in the shower:
One hand to hold the bag under me, and the other using the turkey baster. Then shower and get into position:
Look at an image of the colon:
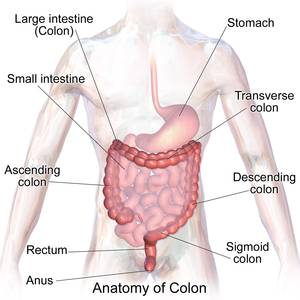
to understand which positions to lie in afterwards to get it to flow through the whole colon. Adding enough water/saline to make it flow easy is important. The more you can elevate your hips at first, the better. An inversion table works great. You can also do yoga-type positions like this:

And/or decline yourself off a couch/bed with your hips on the bed and your head on the floor.

Try to hold it in overnight. You can use Imodium if needed. Once you get the liquid to the right side of the colon you can stay in that position overnight or slowly revert to a standing position and from there gravity should keep the liquid at the cecum. If you keep it there it should reabsorb.
Regarding how long to stay in each position while trying to get it to flow through the whole colon depends on a variety of factors, including how much liquid you've added, whether your colon is cleared out, whether a person has structural defects in their colon, etc. I generally do the retention enema after a BM (when colon is most empty) and use about 3-5 turkey basters worth (each baster is about 1.75 fl oz/52ml) and can feel the liquid flow into the top of my colon within ~10 seconds of being up side down on inversion table. In other cases you might have to lie on each side for ~15 minutes.
Here's some discussion about a 2023 study of 8 people where they compared this method to colonoscopy and found that 50% of subjects failed to get the liquid all the way to their cecum. https://forum.humanmicrobiome.info/threads/colonic-distribution-of-fmt-by-different-enema-procedures-compared-to.187/
--
Why you should use a turkey baster + gravity instead of other methods with tubes:
- This method is more simple and quick. No need for more complicated ones.
- It gets the entire colon. If you use tubing methods without gravity you will not get the whole colon.
- Tubes are an unnecessary risk (scraping, perforation, detachment).
- Smaller width = gets blocked/clogged easier, and thus requires filtering/straining which simply takes up unnecessary time and increases oxygen exposure.
Diet:
Diet's role in FMT is not established.
A few studies showed that FMT success depends on changing bile acid metabolism [1], and this is very much inline with my own experiences. I did not notice a major impact from donor diet, except for when one donor ate nuts (which harm me), they were not fully digested and the undigested nuts in their stool also harmed me.
This 2017 article says OpenBiome said "their own data suggests that diet has no bearing on whether or not an otherwise healthy individual gives successful stool". The data was presented at this DDW conference then published in this abstract.
A small 2016 study concluded that patients with successful FMT for c. diff reported higher fruit and fiber consumption, compared to patients who's FMTs failed.
Donor composition and fiber promote strain engraftment in a randomized controlled trial of fecal microbiota transplant for ulcerative colitis (Jun 2025, n=27) "the effect depends on the specific donor microbiota and not on patient fiber use" https://forum.humanmicrobiome.info/threads/donor-composition-and-fiber-promote-strain-engraftment-in-a-randomized.1060/
Prebiotics and other whole foods that harmed me prior to FMT also harmed me during & after FMT with ineffective donors. I do not think you should/can introduce previously unsafe foods until you're pretty much in complete recovery. My experience with this says it is misguided to try and feed the new bacteria from the FMT. In my opinion you should continue to eat the foods which were the most beneficial to you prior to FMT. And also be aware that low quality donors may cause you to develop new food intolerances.
This 2021 study showed no benefit from fasting beforehand.
In cases of bile acid metabolism issues (which can cause a variety of things including diarrhea), a certain donor was able to correct/greatly improve that without doing anything special, when other donors had no impact. Donor quality seems to be the #1 factor for everything.
Fecal Microbiota Transplantation Combined with a Low FODMAP Diet for the Treatment of Irritable Bowel Syndrome with Predominant Diarrhea (Sep 2022) https://www.hindawi.com/journals/omcl/2022/5121496/ "LFD enhanced the efficacy of FMT, increased the gut microbial diversity after FMT, and strengthened the inhibitory effect of FMT on conditional pathogens"
Weak evidence indicating that the donor and recipient should both eat a healthy diet: https://forum.humanmicrobiome.info/threads/faecal-transplantation-for-ulcerative-colitis-from-diet-conditioned-do.435/ Faecal Transplantation for Ulcerative Colitis From Diet Conditioned Donors Followed by Dietary Intervention Results in Favourable Gut Microbial Profile Compared to Faecal Transplantation Alone (May 2024, n=21)
Donor diet:
Vegetarians have fewer pathogens (Thai study): https://www.jmb.or.kr/journal/viewJournal.html?doi=10.4014/jmb.1603.03057
Worse inflammatory profile in omnivores than in vegetarians associates with the gut microbiota composition: https://dmsjournal.biomedcentral.com/articles/10.1186/s13098-017-0261-x
Sep 2021 study with 8 donors and 62 patients found no impact from donor diet.
Scientific info:
Review, Jan 2015: Wide benefit from fecal transplants https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4284325/
Review, Mar 2016: Fecal Microbiota Transplantation: Current Applications, Effectiveness, and Future Perspectives https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4895930/
Review, Mar 2017: Novel Indications for Fecal Microbial Transplantation: Update and Review of the Literature https://link.springer.com/article/10.1007%2Fs10620-017-4535-9
Review, Jan 2021: Fecal Microbiota Transplantation: A New Therapeutic Attempt from the Gut to the Brain https://www.hindawi.com/journals/grp/2021/6699268/
Guidelines: European consensus conference on faecal microbiota transplantation in clinical practice (2017): https://gut.bmj.com/content/66/4/569
Swiss expert opinion: current approaches in faecal microbiota transplantation in daily practice (2023) https://smw.ch/index.php/smw/article/view/3472/5739
Guidelines: The use of faecal microbiota transplant as treatment for recurrent or refractory Clostridium difficile infection and other potential indications: joint British Society of Gastroenterology (BSG) and Healthcare Infection Society (HIS) guidelines (2018): https://dx.doi.org/10.1136/gutjnl-2018-316818
Review, Jan 2019: Systematic review with meta‐analysis: review of donor features, procedures and outcomes in 168 clinical studies of faecal microbiota transplantation: https://onlinelibrary.wiley.com/doi/abs/10.1111/apt.15116
Methodology/procedure:
FMT methodology has major impact. FMT with patient's own feces results in significant changes. Possibly due to exposure to aerobic conditions. High rate of adverse events in this group: https://www.gastrojournal.org/article/S0016-5085%2815%2901581-4/fulltext
Breakthrough study that took us from being able to culture only 1% of gut microbes to >70% did so by adhering to strict anaerobic conditions: https://www.the-scientist.com/?articles.view/articleNo/46019/title/Most-Gut-Microbes-Can-Be-Cultured – https://www.nature.com/nature/journal/v533/n7604/full/nature17645.html
Oxygen tolerance of anaerobic bacteria isolated from human feces (1989): "Thirty O2-intolerant bacterial strains that reached 100% mortality after 120 min of air exposure were isolated. Ten of these strains were tested for their atmospheric O2 sensitivity as a function of air exposure time; all tested microorganisms showed a similar mortality trend on exposure to air. In fact, 50% of cells survive, on the average, after 4–5 min of atmospheric O2; this percentage decreases to 3–5% after only 20 min, and after 40 min only one cell in a thousand survives; all strains reached 100% mortality in a time range of 100–120 min." https://link.springer.com/article/10.1007/BF01568901
2017 OpenBiome/MIT study confirms that oxygen exposure is the most important factor to reduce during processing: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0170922
Contradictory 2018 result from Japanese researchers showing Anaerobic Stool Preparation Method for Fecal Microbiota Transplantation Is Not Superior to Conventional Aerobic Method in Preserving Anaerobic Bacteria: https://journals.lww.com/ajg/Fulltext/2018/02001/Anaerobic_Stool_Preparation_Method_for_Fecal.125.aspx
Another contradictory result: "Fairly surprisingly but in line with our previous results which downplayed the effect of atmosphere on integrity of waiting samples, we found that oxygen exclusion during transplant manufacturing was not an essential prerequisite for ensuring survival of most bacterial populations, at least in rapidly conditioned stool suspensions. The precautions highlighted would hence allow to benefit from stools inherent reducing capacity to protect most oxygen-sensitive bacterial taxa of the Firmicutes phylum." (2019) https://www.nature.com/articles/s41598-019-45173-4
Feb 2019: https://doi.org/10.1016/j.ebiom.2019.02.023 "The practice of preparing material for faecal transplantation in ambient air profoundly affects viable microbial content, disproportionately reducing the abundance of anaerobic commensals and the capacity for biosynthesis of important anti-inflammatory metabolites. In contrast, while reducing overall levels of viable bacteria, freeze-thaw did not significantly alter viable microbiota composition." Critique of this paper.
Stool preparation under anaerobic conditions contributes to retention of obligate anaerobes: potential improvement for fecal microbiota transplantation (Oct 2021) https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-021-02325-9
Impact of Different Fecal Processing Methods (homogenization & freezing) on Assessments of Bacterial Diversity in the Human Intestine (2016): https://journal.frontiersin.org/article/10.3389/fmicb.2016.01643/full
A Guide for Ex Vivo Handling and Storage of Stool Samples Intended for Fecal Microbiota Transplantation (June 2019) https://www.nature.com/articles/s41598-019-45173-4 "if time before transformation to transplants would exceed 24 hours (up to 72), fresh samples should not be exposed to temperatures above 20 °C (68 °F), and refrigeration at 4 °C (39 °F) can be a safe solution. Removing air above collected samples was sufficient to preserve viability. Maltodextrin-trehalose containing cryoprotectants most effective. Rapid (37°C, 98.6°F) thawing > slow thaw"
"Following 72 hours of storage, faecal microbial composition was assessed by 16 S rRNA amplicon sequencing. Refrigeration was associated with no significant alteration in faecal microbiota diversity or composition" (2015) https://www.nature.com/articles/srep16350
"The bacterial diversity of the fecal flora and the total number of bacteria were significantly reduced after 8 and 24 hours at both room temperature and 4°C" https://www.sciencedirect.com/science/article/abs/pii/S0732889304001774
"Longer durations of stool processing time, up to 3 hours, does not appear to promote a pathological microbial bloom or impact donor FMT effectiveness in CDI" - (Openbiome, 2017). Confirmed in 2020, again for C. Diff, along with storage duration of up to 520 days [1].
Impact of time and temperature on gut microbiota and SCFA composition in stool samples (Aug 2020, n=10) https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0236944 "values obtained for methanogens, L. reuteri and total bacteria are still representative even after storage for up to 48 hours at room temperature (20°C) or 4°C. The overall microbial composition and structure appeared to be influenced more by laboratory errors introduced during sample processing than by the actual effects of temperature and time. Although microbial activity was demonstrated by elevated SCFA at both 4°C and RT, SCFAs ratios were more stable over the different conditions"
"several measures of alpha diversity, relative abundance, and overall community composition are robust to storage at 4 °C for up to 96 h. The greatest change in community composition occurred between 0 and 24 h of storage" (Dec 2021) https://gutpathogens.biomedcentral.com/articles/10.1186/s13099-021-00470-0
2020 study with 100 patients compared Openbiome's 23g of frozen fecal preparation delivered via lower route, vs 30-50g fresh stool obtained from patient-identified donors. Openbiome had an 86% success rate compared to 100% from fresh patient stool https://link.springer.com/article/10.1007/s10620-020-06459-0
Meta Analysis and Systematic Review, Dec 2019: Proton pump inhibitor in upper gastrointestinal fecal microbiota transplant: A systematic review and analysis https://onlinelibrary.wiley.com/doi/10.1111/jgh.14958 "We did not find evidence supporting a clinically significant benefit from routine use of PPIs in FMT protocol"
4-7 size 00 non-coated gelatine capsules, with no glycerol, stored in regular freezer was still effective for c. diff after a year (Jun 2021) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8213398/
Purified fecal matter had lower rates of adverse events vs crude fecal matter. No significant difference in the rate of clinical response or clinical remission between the two groups of different methods. (2018): https://link.springer.com/article/10.1007%2Fs12325-018-0800-3 The Safety of Fecal Microbiota Transplantation for Crohn’s Disease: Findings from A Long-Term Study
Freezing:
"The results in individual studies are somewhat mixed, with some finding improved preservation without any buffer (cryoprotectant)" https://forum.humanmicrobiome.info/threads/antifreeze-in-stool-fmt-capsules-glycerol-vs-maltodextrin-80-medical-f.413/post-1204 - Cites these two studies: Functional amplification and preservation of human gut microbiota (2017), Comparative methods for fecal sample storage to preserve gut microbial structure and function in an in vitro model of the human colon (2020).
"Changes induced in fecal microbiota with different storage conditions are marginal compared to the variations between horses" (2024) https://forum.humanmicrobiome.info/threads/assessment-of-fecal-bacterial-viability-and-diversity-in-fresh-and-fro.482/
Fresh Versus Frozen Stool for Fecal Microbiota Transplantation—Assessment by Multimethod Approach Combining Culturing, Flow Cytometry, and Next-Generation Sequencing (Jul 2022) https://www.frontiersin.org/articles/10.3389/fmicb.2022.872735/full "unknown fraction becoming the dominant one, with an average contribution of 57.47% per sample. It will be very interesting to uncover what this unknown fraction is (e.g., bacterial spores), as this may change our conclusions (if these are spores, the viability could be even higher after freezing). Our results clearly show that whole stool freezing without any cryoprotectants has a great impact on the cultivability and biodiversity of the bacterial community, and possibly also on the viability of bacterial cells."
Prolonged storage reduces viability of Peptacetobacter (Clostridium) hiranonis and core intestinal bacteria in fecal microbiota transplantation preparations for dogs (Jan 2025) https://www.frontiersin.org/journals/microbiology/articles/10.3389/fmicb.2024.1502452/full - glycerol preserves better than lyophilized or no cryoprotectant.
El-Salhy's highly effective 2019 IBS FMT trial had the donor store the stool in their home -20°C freezer. They were then slow thawed at 4°C for 2 days before transplantation.
Long-term storage of feces at −80 °C versus −20 °C is negligible for 16S rRNA amplicon profiling of the equine bacterial microbiome (Mar 2021, 4 years) https://peerj.com/articles/10837/ "adding to accumulating evidence indicating that standard domestic freezers are both economical and effective for microbiome research"
4-7 size 00 non-coated gelatine capsules, with no glycerol, stored in regular freezer was still effective for c. diff after a year (Jun 2021) https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8213398/
Interpersonal Variations in Gut Microbiota Profiles Supersedes the Effects of Differing Fecal Storage Conditions (2018) https://www.nature.com/articles/s41598-018-35843-0 "fecal samples can efficiently be stored in −20 °C freezers or in one of the presented storage buffers, without severe alterations in bacterial composition"
Effects of the long-term storage of human fecal microbiota samples collected in RNAlater (2019): https://www.nature.com/articles/s41598-018-36953-5 "Overall, long-term stool storage at -80 °C had only limited effects on the microbiota composition of human feces"
Freezing changes ratio of Firmicutes to Bacteroides: https://microbiomethod.blogspot.co.uk/2016/11/sampling-storing-and-extracting-dna.html and https://www.ijidonline.com/article/S1201-9712(18)33883-9/abstract Standardization of gut microbiota analysis: Variability in samples taken at different times from single case and the effect of the freezing the sample (2018)
Improved Preservation of Treponema pallidum and Other Bacteria by Freezing with Glycerol (1954): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1056982 - Bacteria amounts are cut in almost half after just one freezing and thawing cycle if they are without glycerol, but the amount lost is negligible if stored in a 15% glycerol suspension. Least amount of damage when rapidly frozen and rapidly thawed.
Maltodextrin and trehalose as alternatives to glycerol (Jun 2019): https://www.nature.com/articles/s41598-019-45173-4
Freeze drying: (lyophilization) One study showed that for c.diff: Fresh > flash freeze > lyophilised (2017). Others have concluded that freeze drying is not significantly worse (2016), (2020), (2024).
Another showed no difference from fresh vs frozen: Simple faecal preparation and efficacy of frozen inoculum in faecal microbiota transplantation for recurrent Clostridium difficile infection – an observational cohort study (2014): https://doi.org/10.1111/apt.13009
Is frozen fecal microbiota transplantation as effective as fresh fecal microbiota transplantation in patients with recurrent or refractory Clostridium difficile infection: A meta-analysis? (2017): https://doi.org/10.1016/j.diagmicrobio.2017.05.007 - no statistical difference.
For IBD: "my colleagues and I used both fresh and frozen stool in our study, and both types seemed to work" https://www.gastroenterologyandhepatology.net/archives/may-2018/update-on-fecal-microbiota-transplantation-in-patients-with-inflammatory-bowel-disease/
Mar 2020 Systematic Review and Meta-Analysis of c. diff trials concluded no difference between fresh and frozen. 2022 Systematic Review and Network Meta-analysis found no difference for Fresh Versus Frozen Versus Lyophilized for C. Diff.
Impact of Fecal Microbiota Transplant Formulations, Storage Conditions, and Duration on Bacterial Viability, Functionality, and Clinical Outcomes in Patients with Recurrent Clostridioides difficile Infection (Mar 2025) https://www.mdpi.com/2076-2607/13/3/587 "Clinical success rates in 537 rCDI patients were not significantly different among the three formulations. However, longer storage durations and advanced recipient age negatively impacted clinical efficacy"
Feb 2021 study tested engraftment using a maltodextrin:trehalose cocktail mixed with human feces, transplanted to germ-free mice, and found it was better than saline-only, but still worse than fresh.
Effects of Different Treatment of Fecal Microbiota Transplantation Techniques on Treatment of Ulcerative Colitis in Rats (Jul 2021, 10% glycerol) https://www.frontiersin.org/articles/10.3389/fmicb.2021.683234/full "FMT is a feasible method for treating UC, with frozen FMT having a superior therapeutic effect than that of fresh FMT"
A Systematic Review and Meta-Analysis of Randomized Controlled Trials of Fecal Microbiota Transplantation for the Treatment of Inflammatory Bowel Disease (Jun 2022) https://www.hindawi.com/journals/ecam/2022/8266793/ "higher clinical remission for fresh fecal FMT (40.9%) than that for frozen fecal FMT (32.2%)"
Dose:
This 2017 review comments on a C. diff study where a small dose (few capsules) was as effective as much larger doses: https://www.tandfonline.com/doi/full/10.1080/19490976.2017.1316447 - this is in line with my own experiences.
Jan 2019 Q&A/overview of IBD studies mentions that low doses were as effective or more effective than larger ones: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6423689/
This 2014 review highlights one or more studies that found the opposite: efficacy was increased after increasing dose from 20 grams to 40 grams. And also says that it seemed at the time that rectal administration was more effective than oral. https://web.archive.org/web/20180802200322/https://webcache.googleusercontent.com/search?q=cache:92IjXZvAswIJ:https://www.omicsonline.org/open-access/upper-versus-lower-gastrointestinal-route-of-fecal-microbiota-transplantation-in-the-treatment-of-clostridium-difficile-infection-2161-069X-4-169.php
Efficacy of faecal microbiota transplantation for patients with irritable bowel syndrome in a randomised, double-blind, placebo-controlled study (Dec 2019, n=165) https://gut.bmj.com/content/69/5/859 "89% response rate in patients who received 60g FMT. The response to FMT increased with the dose (30g vs 60g). The use of a superdonor is necessary for successful FMT"
Increasing the Dose and/or Repeating Faecal Microbiota Transplantation (FMT) Increases the Response in Patients with Irritable Bowel Syndrome (IBS) (June 2019) https://www.mdpi.com/2072-6643/11/6/1415/htm - another in 2023.
Following their first FMT treatment, 699 patients (60%) were cured. After repeated FMT treatments, 944 patients (81%) were cured. (Jun 2025, n=1170) Clinical management of Clostridioides difficile infection with faecal microbiota transplantation: a real-world cohort study. https://www.thelancet.com/journals/eclinm/article/PIIS2589-5370(25)00234-2/fulltext
Frequency:
We then compared four different strategies based on the frequency of FMT over four weeks: (1) twice a week; (2) once a week; (3) two FMTs; (4) one FMT. We were able to transfer human bacteria to mice, irrespective of the strategy used. We detected human bacteria after four weeks, even if only one FMT was performed, but there was a shift of the microbiota over time. FMT twice a week for four weeks was too frequent and perturbed the stability of the newly formed ecosystem. FMT once a week appears to be the best compromise as it allowed engraftment of Faecalibacterium, and a higher diversity of bacteria belonging to the Bacteroidales order. FMT was given orally. (2018): https://www.nature.com/articles/s41598-018-25300-3
For UC/IBD: "As for the frequency of FMT administration, once a week seemed to work in our study. The efficacy was similar in the Australian studies, in which FMT was performed 5 times a week for 8 weeks. Therefore, I think that FMT definitely needs to be given more than once, probably repeatedly over at least 6 weeks, unlike with C difficile infection" https://www.gastroenterologyandhepatology.net/archives/may-2018/update-on-fecal-microbiota-transplantation-in-patients-with-inflammatory-bowel-disease/
Personal experience: With the best donors I used it seemed like I needed a daily dose for a long period of time. Recently I tested a 1x/week dose and was not impressed. It might be ok for a maintenance dose, but not more than that.
Impact factors:
Supporting evidence for young athletes being better donors:
Athletes have higher diversity, and their gut microbiome differs at the functional metabolic level. There is a direct connection with the mitochondria [1][2]. Differences in professional martial arts athletes between different competition levels (Dec 2019).
Endurance exercise and gut microbiota: A review (2017). 2020 review. Grip strength [1][2-4][5], muscle mass, strength, and reaction time as vital signs. Physical fitness is associated with better brain structure and brain functioning. Athletes have healthier brains and can better process external sounds (2019).
Cardiorespiratory fitness is correlated with increased microbial diversity [1][2][3][4]. Gut Microbiota Composition is Related to Cardiorespiratory Fitness [1][2]. High-intensity swimming during the pre-competition period can increase bacterial diversity (May 2022, n=24).
2017 review, Exercise Modifies the Gut Microbiota with Positive Health Effects. Sports medicine review. Gut microbiome regulates skeletal muscle mass and function [1]. Long-term high loading intensity of aerobic exercise improves skeletal muscle performance via the gut microbiota-testosterone axis (Dec 2022). Article referencing post-lyme FMT done with athlete & follow up study. Another by the same person (Peterson) discussing "poop doping".
There have been lots of articles, such as this one, on Jonathan Scheiman's Harvard lab which is studying athletes poop/gut microbiomes in regards to athletic performance. Their June 2019 study found a performance enhancing microbe (Veillonella atypica).
Fecal microbiota transplantation confers beneficial metabolic effects of diet and exercise on diet-induced obese mice. More in 2025: [Jan 2025], [Feb 2025]. Another in 2023 pointing to bile acid metabolism as a mechanism. Grip strength and muscle mass transferable via FMT [1].
Mice given FMT from elite cyclists and soccer players had increased energy stores (Mar 2025) https://forum.humanmicrobiome.info/threads/mice-given-fmt-from-elite-cyclists-and-soccer-players-had-increased-en.930/ Atypical gut microbial ecosystem from athletes with very high exercise capacity improves insulin sensitivity and muscle glycogen store in mice.
Donor selection:
Forum threads related to donor quality: https://forum.humanmicrobiome.info/tags/donor-quality/
The discussion section of this 2014 review paper "Rural and urban microbiota - To be or not to be?" provides excellent info on gut microbiome, FMT, and donor selection: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4153773/
Microbial determinants of effective donors in faecal microbiota transplantation for UC (Jul 2022) https://gut.bmj.com/content/72/1/90 "one donor having 100% efficacy compared with a second donor (36% efficacy). Donor microbiota stability and species evenness were identified as novel metrics that were associated with therapeutic efficacy in UC, beyond individual microbial species or metabolites"
Donor species richness determines FMT success for IBD (2015): https://doi.org/10.1093/ecco-jcc/jjv203 | The taxonomic composition of the donor intestinal microbiota is a major factor influencing the efficacy of faecal microbiota transplantation in therapy refractory ulcerative colitis (2017): https://onlinelibrary.wiley.com/doi/10.1111/apt.14387/abstract
Systematic review of donor and recipient predictive biomarkers of response to faecal microbiota transplantation in patients with ulcerative colitis (May 2022) https://www.thelancet.com/journals/ebiom/article/PIIS2352-3964(22)00269-9/fulltext
Irritable Bowel Syndrome-Like Symptoms Following Fecal Microbiota Transplantation: A Possible Donor-Dependent Complication (2017): https://sci-hub.se/10.1038/ajg.2016.472
One UC/IBD study showed "Stool from one donor appeared to do much better than from the others" https://www.gastroenterologyandhepatology.net/archives/may-2018/update-on-fecal-microbiota-transplantation-in-patients-with-inflammatory-bowel-disease/
According to their safety publications, OpenBiome has at least 1 donor with a 100% efficacy rate after more than 100 patients, while most of their other donors seem to be around 80%. This supports the notion that donor quality is the most important factor: https://forum.humanmicrobiome.info/threads/analysis-of-openbiomes-safety-and-efficacy-aug-2018.55/
Fecal Microbiota Transplantation engraftment after budesonide or placebo in patients with active ulcerative colitis using pre-selected donors: a randomized pilot study (Apr 2024, n=24) https://forum.humanmicrobiome.info/threads/fecal-microbiota-transplantation-engraftment-after-budesonide-or-place.337/ "Clinical response appeared donor-dependent. These findings also suggest that selecting FMT donors based on in vitro, microbiome community, or animal model data alone may be insufficient to predict FMT clinical response"
Rigorous Donor Selection for Fecal Microbiota Transplantation in Active Ulcerative Colitis: Key Lessons From a Randomized Controlled Trial Halted for Futility (May 2024, n=72) https://forum.humanmicrobiome.info/threads/rigorous-donor-selection-for-fecal-microbiota-transplantation-in-activ.603/ "donor material was selected after a rigorous screening based on microbial cell count, enterotype, and the abundance of specific genera"
Donor-recipient matching:
Donor matching vs niches. Opinion on article titled "Could Donor Matching Help Fecal Transplants to Work Better?" Study: MHC variation sculpts individualized microbial communities that control susceptibility to enteric infection (2015) https://forum.humanmicrobiome.info/threads/donor-matching-vs-niches-opinion-on-article-titled-could-donor-matchin.136/
Recipient factors in faecal microbiota transplantation: one stool does not fit all (Apr 2021) https://www.nature.com/articles/s41575-021-00441-5 - https://archive.ph/HNnE2#selection-2641.12-2641.13 - their abstract and conclusions are nowhere near as bold as their title. I don't disagree with their abstract and conclusion at all. But I would object to their "one stool does not fit all" title, since that is far from being proven, and will not be till someone tests the type of donor I've been advocating & searching for for years.
A new compatibility test for donor selection for faecal microbiota transplantation in ulcerative colitis (Jan 2017) https://academic.oup.com/ecco-jcc/article/11/suppl_1/S480/2961722
The interplay of gut microbiota between donors and recipients determines the efficacy of fecal microbiota transplantation (Jul 2022) https://www.tandfonline.com/doi/full/10.1080/19490976.2022.2100197
The trans-kingdom battle between donor and recipient gut microbiome influences fecal microbiota transplantation outcome (Oct 2020) https://www.nature.com/articles/s41598-020-75162-x
Microbial Strain Engraftment, Persistence and Replacement after Fecal Microbiota Transplantation (Sep 2020) https://web.archive.org/web/20220722025942/https://old.reddit.com/r/HumanMicrobiome/comments/w4zfbm/microbial_strain_engraftment_persistence_and/
Evidence opposing the need for sex-matching:
Fecal Microbiota Transplantation Reduces Symptoms in Some Patients With Irritable Bowel Syndrome with Predominant Abdominal Bloating: Short- and Long-Term Results from a Placebo-Controlled Randomized Trial (Jul 2020, n=62) https://forum.humanmicrobiome.info/threads/fecal-microbiota-transplantation-reduces-symptoms-in-some-patients-wit.273/ - donors were men. Women recipients had better responses.
Evidence supporting the need for sex-matching:
The Effect of Cross-Sex Fecal Microbiota Transplantation on Metabolism and Hormonal Status in Adult Rats (Jan 2024) https://forum.humanmicrobiome.info/threads/the-effect-of-cross-sex-fecal-microbiota-transplantation-on-metabolism.234/ "cross-sex male recipients displayed a significantly lower testosterone concentration compared to the males that received same-sex FMT"
Misc:
FUT2 genotype and secretory status are not associated with fecal microbial composition and inferred function in healthy subjects (2018): https://doi.org/10.1080/19490976.2018.1445956
FMT success may depend on changing bile acid metabolism: https://humanmicrobiome.info/bile
"Instead of a focus on restoring secondary bile acid generation, restoring the organisms that produce 5-aminovalerate or consume proline / glycine are more important" https://journals.plos.org/plospathogens/article?id=10.1371/journal.ppat.1010015 Bile acid-independent protection against Clostridioides difficile infection (Oct 2021, mice)
Gut fungal composition of both donors and recipients: https://humanmicrobiome.info/candida#fmt
"the host’s inflammatory immune status can limit the efficacy of microbiota-based therapeutics to treat C. difficile infection" (Feb 2021, mice) https://www.nature.com/articles/s41467-020-20793-x
Antibiotic use 3–12 months before donation decreased the effectiveness of FMT. Stool with a Bristol Stool Scale score of 4 and 5 or above showed improved FMT effectiveness for C. diff. Donor sex, BMI, smoking status, H pylori carriage, birth mode, total donation weight, and donor−recipient sex concordance did not affect FMT outcomes. https://forum.humanmicrobiome.info/threads/effects-of-clinical-donor-characteristics-on-the-success-of-faecal-mic.894/
Pooled stools (multiple donors) can be more effective [1].
Saliva may have beneficial impacts [1][2].
May 2017, OpenBiome presented data on donor efficacy factors and pediatric access at DDW. The nonprofit stool bank shared data from a 1,413 patient cohort of fecal transplant recipients and research from 14 abstracts at Digestive Disease Week. https://www.openbiome.org/press-releases/2017/5/23/openbiome-presented-data-on-donor-efficacy-factors-and-pediatric-access-at-ddw
Age:
More: https://humanmicrobiome.info/aging/
A few limited studies suggest infant stool can be viable for FMT. Anecdotes of failures might be due to the infant inheriting dysbiosis from the mother/parents.
Postnatal colonization with human "infant-type" Bifidobacterium species alters behavior of adult gnotobiotic mice (2018): http://journals.plos.org/plosone/article?id=10.1371/journal.pone.0196510 - this study is not an FMT study, but closer to a probiotic study since they only used 4 "infant type" bifido. But I haven't seen many studies exploring the effectiveness of infant gut microbes.
Gut Microbes from Healthy Infants Block Milk Allergy Development in Mice. Healthy infants harbor intestinal bacteria that protect against food allergy (2019): https://www.niaid.nih.gov/news-events/gut-microbes-healthy-infants-block-milk-allergy-development-mice - https://doi.org/10.1038/s41591-018-0324-z "gut microbes from healthy human infant donors transplanted into mice protected animals exposed to milk from experiencing allergic reactions, while gut microbes transplanted from infants allergic to milk did not"
Different responses to FMT depending on age of donor (in chickens): https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0163932
Outcomes:
FMT changes to gut microbiome last long-term [1][2][3].
Not all donor microbes colonize the recipient. Two studies in March 2019 looked at which ones colonized [1][2]. Similar 2021 study looking at Long-Term (6 months) Bacterial and Fungal Dynamics. 2020 study finds 38% of FMT-driven changes were strain replacements.
More studies looking at engraftment outcomes and more https://forum.humanmicrobiome.info/threads/variability-of-strain-engraftment-and-predictability-of-microbiome-com.325/post-721 - donors with less engraftment can be more effective.
You can search forum thread titles for "engraftment" for more: https://forum.humanmicrobiome.info/search/553842/?q=engraftment&c[title_only]=1&o=date
Precise quantification of bacterial strains after fecal microbiota transplantation delineates long-term engraftment and explains outcomes (Sep 2021) https://www.nature.com/articles/s41564-021-00966-0
Exploration of Potential Gut Microbiota-Derived Biomarkers to Predict the Success of Fecal Microbiota Transplantation in Ulcerative Colitis: A Prospective Cohort in Korea (Nov 2021, n=10) https://www.gutnliver.org/journal/view.html?doi=10.5009/gnl210369 "nonresponder group had a higher rate of preservation of donor microbiota, underscoring that engraftment degrees are not one of the major drivers for the success of FMT"
"Engraftment of the donors’ microbiota could not be clearly linked with clinical response, possibly because not every donor has an ideal microbiome" https://www.cghjournal.org/article/S1542-3565(24)00907-8/fulltext Gut Microbiota Features in Relation to Fecal Microbiota Transplantation Outcome in Ulcerative Colitis: A Systematic Review and Meta-Analysis (Oct 2024).
Recipient viromes resembled those of their donors for up to 12 months. Tracking individual bacteriophage colonisation revealed that engraftment of individual bacteriophages was dependent on specific donor-recipient pairings. Specifically, multiple recipients from a single donor displayed highly individualised virus colonisation patterns (2018).
Bacteriophages are associated with FMT treatment outcome [2017][2019].
Guts of Fecal Transplant Patients Resemble their Donors' (2016) https://web.archive.org/web/20221203094052/https://www.hcplive.com/view/guts-of-fecal-transplant-patients-resemble-their-donors - https://bmcmedicine.biomedcentral.com/articles/10.1186/s12916-016-0698-z
For IBD: "We now have 4-year data. All 9 patients who went into remission have now relapsed. All but 1 patient chose to undergo FMT again and remission was induced in all but 1 of these patients. Most patients have elected to continue undergoing FMT anywhere between once every 2 weeks to once a month, and most are still in remission with this approach." https://www.gastroenterologyandhepatology.net/archives/may-2018/update-on-fecal-microbiota-transplantation-in-patients-with-inflammatory-bowel-disease/
ASU autism study 2 year follow up sees nearly 50% reduction in symptoms (April 2019): https://asunow.asu.edu/20190409-discoveries-autism-symptoms-reduced-nearly-50-percent-two-years-after-fecal-transplant
Magdy El-Salhy's IBS study: "Most of the IBS patients maintained a response at 1 year after FMT. Moreover, the improvements in symptoms and quality of life increased over time" https://onlinelibrary.wiley.com/doi/10.1111/nmo.14200 | 3 year follow up.
Intestinal microbiota could transfer host Gut characteristics from pigs to mice [1], but not between mice & zebrafish [2]. "Failure of human-to-mouse FMT to recapitulate the precise microbial contents of the human donors" https://sci-hub.se/https://www.nature.com/articles/s41435-018-0024-1
FMT can transfer not only microbiota but also the donors’ intestinal innate immune status and improved intestinal integrity: https://www.nature.com/articles/srep38599 | But may not completely restore immune function damaged by antibiotics (2017): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5395657/
"By profiling bacteria coated with IgA, we identified IgA-coated bacteria associated with inflammation, and we found that microbial interactions with the host immune system can be transferred across people. This transfer of immune function is likely critical for gut microbiome therapeutics for immune-related diseases." (May 2019) https://www.biorxiv.org/content/10.1101/649384v1.full. Dynamic colonization of microbes and their functions after fecal microbiota transplantation for inflammatory bowel disease.
Fecal Calprotectin and Fecal Indole Predicts Outcome of Fecal Microbiota Transplantation in Subjects with Recurrent Clostridium difficile Infection (Mar 2019): https://www.sciencedirect.com/science/article/pii/S1075996419300459 "low calprotectin and high indole is associated with successful FMT in RCDI in both IBD positive and negative patients. We suggest that the ratio of calprotectin/indole should be evaluated for predicting outcome in FMT in RCDI"
Distinct Fecal and Plasma Metabolites in Children with Autism Spectrum Disorders and Their Modulation after Microbiota Transfer Therapy (Oct 2020) https://msphere.asm.org/content/5/5/e00314-20 "Our results provide evidence that changes in metabolites are one mechanism of the gut-brain connection mediated by the gut microbiota and offer plausible clinical evidence for a promising autism treatment and biomarkers"
The fecal microbiota transplantation response differs between patients with severe and moderate irritable bowel symptoms (Apr 2022, n=164) https://www.tandfonline.com/doi/full/10.1080/00365521.2022.2064725 "response rates were higher in Severe-IBS patients than in Moderate-IBS patients"
Safety:
Mar 2025: Long-term safety of fecal microbiota transplantation in Chinese children from 2013 to 2023: a single-center retrospective study https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-025-03858-z "This study stands out for its substantial sample size (813), making it’s the largest reported series in pediatrics, as well as for having the longest follow-up period for FMT in this population"
Sep 2023: Long-Term Safety Outcomes of Fecal Microbiota Transplantation: Real-World Data Over 8 Years From the Hong Kong FMT Registry https://www.cghjournal.org/article/S1542-3565(23)00712-7/abstract "FMT has an excellent long-term safety profile. The risk of developing new medical conditions beyond 12 months after FMT is low"
Sep 2022: The Global Incidence of Adverse Events Associated with Fecal Microbiota Transplantation in Children over the Past 20 Years: A Systematic Review and Meta-Analysis https://onlinelibrary.wiley.com/doi/10.1111/jgh.15996 "Adverse events related to FMT in children are mostly mild to moderate, of short duration, and self-limiting. Therefore, the use of FMT in children is safe and worthy of widespread promotion. There was no difference in the incidence of adverse events between the upper and lower gastrointestinal tracts"
Feb 2022: Adverse events in fecal microbiota transplantation: a systematic review and meta-analysis https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8922263/
Jan 2022: Fecal Microbiota Transplant for Clostridioides Difficile Infection Is Safe and Efficacious in an Immunocompromised Cohort https://link.springer.com/article/10.1007%2Fs10620-021-07347-x
Aug 2021: Systematic review with meta-analysis: encapsulated faecal microbiota transplantation – evidence for clinical efficacy https://journals.sagepub.com/doi/10.1177/17562848211041004 "Encapsulated FMT is an effective and safe treatment of rCDI, with cure rates comparable to FMT delivered through other routes"
Jul 2021: Adverse events of fecal microbiota transplantation: a meta-analysis of high-quality studies https://pubmed.ncbi.nlm.nih.gov/34815646/
Jan 2021: Oral Fecal Microbiota Transplant Capsules Are Safe and Effective for Recurrent Clostridioides difficile Infection A Systematic Review and Meta-Analysis https://journals.lww.com/jcge/Abstract/9000/Oral_Fecal_Microbiota_Transplant_Capsules_Are_Safe.97483.aspx "We found an overall efficacy of 82.1% with a low rate of serious adverse events"
Nov 2020: Systematic review: the global incidence of faecal microbiota transplantation‐related adverse events from 2000 to 2020 https://onlinelibrary.wiley.com/doi/abs/10.1111/apt.16148
Oct 2020: AGA releases largest real-world report on safety and effectiveness of fecal microbiota transplantation (FMT). Ninety percent of patients tracked in the AGA FMT National Registry were cured of C. difficile infection with few serious side effects. https://gastro.org/press-releases/aga-releases-largest-real-world-report-on-safety-and-effectiveness-of-fecal-microbiota-transplantation-fmt-2/
Mar 2019: Adjunctive fecal microbiota transplantation in supportive oncology: Emerging indications and considerations in immunocompromised patients: https://www.ebiomedicine.com/article/S2352-3964(19)30215-4/fulltext "Limited available evidence supports the notion that it is a safe therapy in immunocompetent individuals, however further studies are required"
Feb 2019: Clinical Review on the Utility of Fecal Microbiota Transplantation in Immunocompromised Patients. Present literature weighs in favor of FMT in immunocompromised patients, with an acceptable adverse effect profile and minimal risk of infectious adverse events: https://link.springer.com/article/10.1007%2Fs11894-019-0677-6
Jan 2019: Systematic review with meta‐analysis: review of donor features, procedures and outcomes in 168 clinical studies of faecal microbiota transplantation. https://onlinelibrary.wiley.com/doi/abs/10.1111/apt.15116 "Overall adverse event incidence was <1%, mostly GI‐related. Adverse event rates did not differ significantly between routes of FMT administration or indication"
Adverse events in faecal microbiota transplant: a review of the literature (2015): https://doi.org/10.1016/j.jhin.2015.10.024
The long-term effects of faecal microbiota transplantation for gastrointestinal symptoms and general health in patients with recurrent Clostridium difficile infection (2017): https://onlinelibrary.wiley.com/doi/10.1111/apt.14443/abstract
Two documented cases of aspiration pneumonia occurred during upper gastrointestinal tract endoscopy. Similar cases have been identified by other authors (Mar 2019): https://journals.sagepub.com/doi/10.1177/2050640619839918
For IBD: "My colleagues and I have now followed a small number of IBD patients undergoing FMT over 4 years, and no safety concerns have been found" https://www.gastroenterologyandhepatology.net/archives/may-2018/update-on-fecal-microbiota-transplantation-in-patients-with-inflammatory-bowel-disease/
Long-term impact of fecal transplantation in healthy volunteers (Dec 2019, n=3, 15 capsules 2 days in a row, 22g total) "one volunteer developed a fever (102F), with shivers and tachycardia of 102 per minute on the day after administration" https://bmcmicrobiol.biomedcentral.com/articles/10.1186/s12866-019-1689-y - Comment/opinion: these are very common symptoms after FMT, and not a major concern.
Autologous:
FMT with patient's own feces results in significant changes. Possibly due to exposure to aerobic conditions. High rate of adverse events in this group (2015): https://www.gastrojournal.org/article/S0016-5085%2815%2901581-4/fulltext
Review, Feb 2019: Transforming medicine with the microbiome https://archive.fo/IuuPB#selection-1981.0-1997.1 "as microbiomes from individuals who may appear healthy could harbor causal factors of the condition to be treated, resulting in unforeseen resurgence of the disease" https://stm.sciencemag.org/content/11/477/eaaw1815
Review, Jun 2020: Autologous fecal microbiota transplantation for the treatment of inflammatory bowel disease: https://www.sciencedirect.com/science/article/pii/S1931524420301110
Allogenic Fecal Microbiota Transplantation in Patients With Nonalcoholic Fatty Liver Disease Improves Abnormal Small Intestinal Permeability A Randomized Control Trial (May 2020, n=21) https://journals.lww.com/ajg/Abstract/2020/07000/Allogenic_Fecal_Microbiota_Transplantation_in.19.aspx - allogenic (n = 15) or autologous (n = 6). Significant reduction in small intestinal permeability 6 weeks after allogenic FMT. Forty-six potential donors were screened to find 3 suitable donors for this study.
Autologous FMT, collected during the weight loss phase and administrated in the regain phase, might preserve weight loss and glycemic control. (Aug 2020, n=90) Effects of Diet-Modulated Autologous Fecal Microbiota Transplantation on Weight Regain https://archive.vn/WXdFd - no adverse events.
Is Autologous Fecal Microbiota Transfer after Exclusive Enteral Nutrition in Pediatric Crohn’s Disease Patients Rational and Feasible? Data from a Feasibility Test (Apr 2023, n=7) https://www.mdpi.com/2072-6643/15/7/1742 "A high pathogen burden, low-diversity microbiota, and practical deficiencies of EEN-conditioned fecal material might render autologous capsule-FMT an unsuitable approach as maintenance therapy for pediatric CD patients"
Regarding freezing your own stool before antibiotics then using it for auto-FMT afterwards, see the FAQ: https://humanmicrobiome.info/faq/#what-about-autologous-fmt
Sterile fecal filtrate:
Sterile fecal filtrate is effective for treating c.diff (implicating phages) (2016): https://archive.is/gY07m
Comparative effects of fresh and sterile fecal microbiota transplantation in an experimental animal model of necrotizing enterocolitis (Jan 2022) https://www.jpedsurg.org/article/S0022-3468(21)00844-7/fulltext "Fresh and sterile FMT effectively reduced the inflammatory response, oxidative damage, and histological alterations in the gut and brain compared to an experimental NEC model"
Sterile Fecal Filtrate From A Healthy Donor Improves Microbial Diversity In Patients With Hepatic Encephalopathy (July 2023, n=7) https://jgld.ro/jgld/index.php/jgld/article/view/4906 - No improvements to liver function or HE cognition tests.
General FMT articles & videos:
Article covering OpenBiome stool bank, one of their donors, and the need for more donors: https://news.wgbh.org/2017/04/13/science-and-technology/why-central-square-stool-bank-paying-40-poop-donation
Video covering one of OpenBiome's donors: https://www.cnn.com/videos/health/2015/08/25/fecal-transplant-poop-medicine.cnn
VICE coverage of FMT and OpenBiome: https://news.vice.com/story/your-poop-could-save-someones-life
Video coverage of Florida FMT clinic & one of their donors: https://www.youtube.com/watch?v=BxtjWynqW7A
Article covering a clinic in Tampa Florida that helps people do FMT for conditions other than c.diff. They also cover the ASU autism study, safety, and more (Jun 2017): https://www.buzzfeed.com/nidhisubbaraman/inside-tampa-fecal-transplant-clinic
The poo panacea: inside the strange, surprising world of faecal transplants. When treating antibiotic-resistant infections, injecting patients with other people’s excrement can be highly effective. Could it be the answer to dementia, anorexia and obesity too? (Jan 2020) https://www.theguardian.com/lifeandstyle/2020/jan/22/the-poo-panacea-inside-the-strange-surprising-world-of-faecal-transplants
Fecal Transplants May Be a Miracle Cure for Some of Our Nastiest Illnesses (Nov 2016): https://www.wired.com/2016/11/microbiome-therapy-making-fecal-transplants-better/
There is growing evidence faecal transplants could be causing some patients to take on the physical and mental traits of their donors, including body shape and even symptoms of depression (2017): https://www.abc.net.au/news/2017-05-09/faecal-transplant-side-effects-explored-at-conference/8510270
Doctors transfer the power of gut bacteria (Oct 2016): https://azdailysun.com/news/local/doctors-transfer-the-power-of-gut-bacteria/article_5956de37-7b12-52ab-9491-0853b067f39c.html
2017 study shows FMT helpful for Autism: https://medicalxpress.com/news/2017-01-gut-microbe-potential-treatment-autism.html
Article's covering researcher Jeff Leach's microbiome experiments (including DIY FMT) with the Hadza tribe:
- https://www.popsci.com/article/science/scientist-gives-himself-fecal-transplant-try-hunter-gatherers-microbiome
- https://web.archive.org/web/20160601090809/http://humanfoodproject.com/rebecoming-human-happened-day-replaced-99-genes-body-hunter-gatherer/
- https://www.rawstory.com/2017/07/heres-what-happened-to-a-professor-of-genetic-epidemiologys-gut-microbiome-when-he-lived-with-hunter-gatherers/
Article covering researcher Lauren Petersen, who cured herself of post-lyme illness with DIY FMT: https://forum.humanmicrobiome.info/threads/lauren-petersens-diy-fmt-from-an-elite-cyclist-for-chronic-lyme-diseas.597/
Guy does DIY FMT for IBS (does some extreme & unnecessary things): https://forum.humanmicrobiome.info/threads/josiah-zayner-cures-his-ibs-with-diy-fmt-from-a-friend-2016.600/
Thepowerofpoop.com has lots of good & useful info. But also some wrong/outdated info. The blending part of their instructions should be avoided. You don't want to do this since it will kill off a lot of anaerobic microbes (the gut is an anaerobic environment!). And their warning about capsules & SIBO is wrong (see the SIBO section on this page). Haven't vetted their whole site. It looks like the site went down early 2019. You can use archive.org to see old pages.
SIBO:
Some claim using quick release capsules can cause SIBO [1][2]. But it's more likely due to inadequate donor screening/selection. Top-down methods that empty into the stomach or small intestine are common/standard in all types of official and experimental FMT practice [1], and there is no evidence that they cause or worsen "SIBO".
OpenBiome, the main US stool bank (c.diff only) offers all 3 methods (enema, naso tube, capsules): https://www.openbiome.org/fmtcapsules/ - https://www.openbiome.org/clinical-guidance
This 9 person FMT trial that used a nasal tube & tested for SIBO, reported no severe adverse events.
Feb 2021 study showing FMT via capsules can treat SIBO: https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-021-01630-x
The impact of small intestinal bacterial overgrowth on the efficacy of fecal microbiota transplantation in patients with chronic constipation (Aug 2024, n=218) https://forum.humanmicrobiome.info/threads/the-impact-of-small-intestinal-bacterial-overgrowth-on-the-efficacy-of.566/ "efficacy of FMT in the SIBO group was superior"
In ASU's 2017 FMT Autism study they used the oral route (filtered out most of the large particles so no taste, and then mixed it in with liquids that the patients drank) in some patients and rectal in others and found no differences.
This case seems to prove SIBO is a donor problem rather than a "quick release capsule" problem: https://archive.is/ixi6Y - recipient develops SIBO from colon-only FMT.
Naso tube FMT study for IBS symptoms and predominant abdominal bloating see significant improvements https://www.gastrojournal.org/article/S0016-5085(18)30860-6/abstract Fecal Microbiota Transplantation in Irritable Bowel Syndrome with Predominant Abdominal Bloating: Results from a Double Blind, Placebo-Controlled Clinical Trial
Review of 97 patients finds no difference between top and lower routes (2018): https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6305536/
Systematic review with meta‐analysis: review of donor features, procedures and outcomes in 168 clinical studies of faecal microbiota transplantation (Jan 2019) https://onlinelibrary.wiley.com/doi/abs/10.1111/apt.15116 "Overall adverse event incidence was <1%, mostly GI‐related. Adverse event rates did not differ significantly between routes of FMT administration or indication"
Review of 150 patients finds "Small bowel exposure to donor stool was not related to symptoms" (Oct 2019): https://www.ncbi.nlm.nih.gov/pubmed/30882536
Myself and this person had no problems from DIY oral FMT. And I did it many times from multiple donors. I also experimented with lower vs upper route and lower-route-only does not seem to be complete.
FMT Clinics:
Moved to Where to get FMT, since this FMT page was getting too big.
Taymount Clinic
Moved to https://humanmicrobiome.info/where-to-get-fmt/
RDS infusions, Florida
Moved to https://humanmicrobiome.info/where-to-get-fmt/
Center for Digestive Diseases (CDD), AU
Moved to https://humanmicrobiome.info/where-to-get-fmt/
Jason Klop
Moved to https://humanmicrobiome.info/where-to-get-fmt/
Human Microbes
Moved to https://humanmicrobiome.info/where-to-get-fmt/
Microbioma.org:
Moved to https://humanmicrobiome.info/where-to-get-fmt/#microbiomaorg
Experiences:
Experiences and reviews from FMT clinics and other commercial sources of stool donors.
FMT experiences from personal donors.
FMT success stories from thepowerofpoop.com.
Experiences on /r/fecaltransplant.
Communities and forums:
We originated on Reddit, but Reddit has been on a steep decline for years, so we moved to a new forum:
Other groups:
- Facebook group: https://www.facebook.com/groups/FTDonors
- Discord: https://discord.gg/Hnea7fN4vZ
Old subreddits:
- https://old.reddit.com/r/HumanMicrobiome
- https://old.reddit.com/r/fecaltransplant
- https://old.reddit.com/r/FMTClinics
Be very weary of most of the Facebook and Reddit groups. They are riddled with scammers, paid astroturfers, and harmful misinformation. Facebook and Reddit do not police their websites for unethical behavior. They are essentially free-for-alls for scammers, misinformation, and disinformation. The biggest FMT Facebook group is controlled by scammers, as is another one for "FMT for Autism", and another with the URL "facebook.com/groups/fecal.microbiota.transplant", and more. The same group of scammers has raided the /r/FMTClinics sub in the past, and more recently have been branching out all over Reddit. They've engaged in a targeted harassment & disinformation campaign against people who exposed them. It is not difficult to determine "who is right", simply look at the evidence.